Menopause & Perimenopause: A Look at the Impact on Your Tendons
As women transition through the natural phases of life, their bodies undergo significant changes, reshaping the way they experience daily activities and even the way their bodies respond to various stimuli.
Menopause & Perimenopause and the impact on tendons
One often overlooked aspect of this transformation is the profound effect that menopause and perimenopause can have on tendons. These crucial connective tissues, responsible for facilitating movement and supporting joints, are intricately linked to hormonal fluctuations, particularly the drop in estrogen levels.
What is Perimenopause?
Perimenopause, the transitional phase leading up to menopause, heralds a multitude of symptoms including;
- hot flashes
- night sweats
- breast tenderness
- fatigue
- irregular periods
It marks the time when the ovaries cease to ovulate, setting the stage for the next phase.
Menopause
Menopause, on the other hand, is characterized by the complete cessation of periods for a full 12 months.
Understanding the intricate connections between these hormonal changes and their impact on tendons is essential, shedding light on a topic often overlooked in discussions about women’s health.
As you, or the women in your life age, understanding the subtle yet significant ways in which menopause and perimenopause influence tendons is key to receiving adequate treatment.
What are tendons?

Tendons are vital components of the human musculoskeletal system, serving as the attachments between muscles and bones.
As previously mentioned, these fibrous tissues play a fundamental role in our ability to move, acting as attachment points where muscles exert force to create movement.
Tendons not only provide structural support but also absorb the impact generated during high-intensity sports and activities, safeguarding our joints and bones from excessive stress. Their unique properties enable us to perform a wide range of motions.
What are tendons made of?
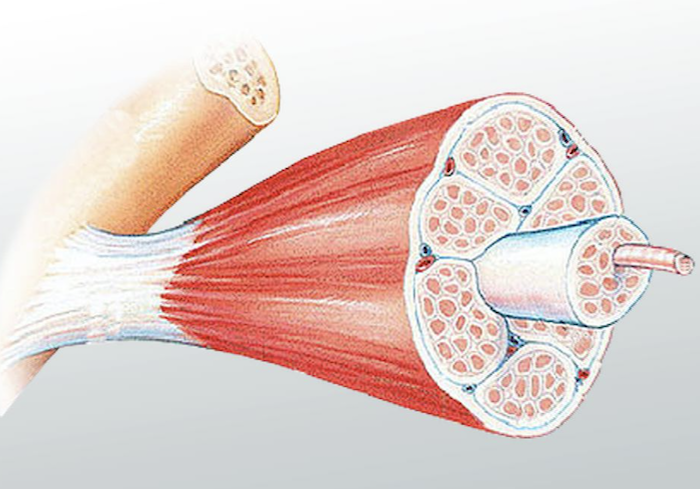
Tendons are primarily composed of collagen, a strong and flexible protein that provides the structural framework for various connective tissues in the body.
These long striations of collagen tissue are tightly packed together, giving tendons their remarkable strength and resilience.
The dense arrangement of collagen fibers enables tendons to withstand significant forces, making them essential for supporting movements, absorbing impact, and ensuring the stability of joints.
What is collagen?
Collagen is a fibrous protein that serves as a fundamental building block in the human body. It is the most abundant protein found in various connective tissues, including tendons, ligaments, skin, bones, and cartilage.
Collagen provides structural support and strength to these tissues, contributing to their elasticity and integrity.
During menopause, when estrogen levels drop, the healing process of tendons can be delayed. This delay occurs because reductions in estrogen lead to a decrease in collagen synthesis and tensile strength, essential factors for the repair and maintenance of these vital connective tissues.
As a result, tendon injuries take longer to heal, necessitating extended recovery periods, especially in post-menopausal individuals.
Strengthening Tendons, What can we do?
Heavy Slow Activity or Load Bearing Exercises
Engaging in weight-bearing exercises, such as weightlifting or resistance training, can help stimulate the production of collagen and strengthen tendons.
Performing these exercises with heavy loads and a slow, controlled pace can promote tendon adaptation and increase their resilience.
Consistent Physical Activity
Regular physical activity, including moderate aerobic exercises like walking or jogging, can enhance blood circulation and promote tendon health.
Incorporating a variety of exercises into the routine can target different muscle groups and tendons, ensuring overall strength and flexibility.
Proper Nutrition
Consuming a balanced diet rich in proteins, vitamins, and minerals is essential for collagen synthesis.
Adequate protein intake provides the necessary building blocks for tendon repair and growth.
Appropriate Warm-up and Stretching
Prior to any physical activity, warming up the body and stretching the muscles and tendons can improve their flexibility and reduce the risk of injury.
Incorporating dynamic stretching exercises into the warm-up routine can specifically target tendons, preparing them for the upcoming activity.
Gradual Progression
When engaging in strength training exercises, it’s vital to progress gradually.
Avoid sudden increases in intensity or duration, as this can strain the tendons and lead to injuries.
Gradual progression allows tendons to adapt to the increasing demands placed upon them, reducing the risk of overuse injuries.
Begin Before Menopause or Early in Menopause
Initiating tendon-strengthening activities before menopause, or at least during the early stages of menopause, is imperative.
Building tendon strength before the hormonal changes associated with menopause occur can provide a solid foundation, making tendons more resilient and better prepared to withstand the challenges that come with age-related hormonal fluctuations.
Significant tendon tears

Significant tendon tears, regardless of age or gender, often can’t be fully repaired. In such cases, the damaged segment of the tendon is dead tissue and cannot be restored. Instead, the focus is shifted to repairing and reinforcing the surrounding healthy tendon tissue to create stable support.
Although complete regeneration is not possible, rehabilitation help optimize the remaining tendon’s function.
Physical therapy and targeted exercises strengthen surrounding muscles and tendons, enabling individuals to regain some mobility and functionality. This also prevents future injury.
What to do with a tendon injury?
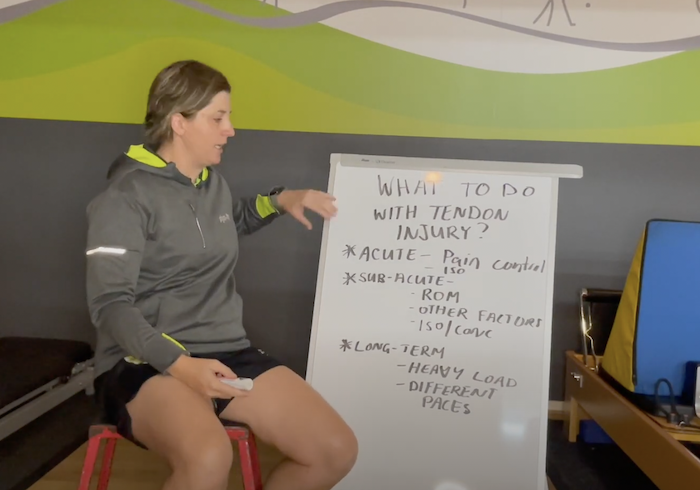
Acute Phase:
During the acute phase of a tendon injury, it is crucial to focus on immediate pain control and symptom management. Individuals often find it challenging to move the affected area due to pain and discomfort.
Nonsteroidal anti-inflammatory drugs (NSAIDs) can be beneficial in alleviating inflammation and pain, although their usage should be carefully considered, taking into account any underlying health conditions.
Additionally, diagnostic scans, such as ultrasounds or MRI, play a pivotal role in providing an accurate assessment of the injury. Isometric exercises, which involve contracting the muscle without changing its length, can be particularly helpful.
These exercises, when performed with controlled, sustained holds and added weights, can effectively reduce pain and promote blood circulation to the injured tendon. It is important to note that experiencing some discomfort during these exercises is normal, as long as the pain diminishes following the workout session.
Subacute Phase:
The subacute phase of a tendon injury, which can extend over several months, requires a more focused and comprehensive approach. Range of movement becomes a primary concern during this period.
Physiotherapists work closely with patients to establish correct movement patterns, especially in cases like shoulder tendinopathy, where proper shoulder blade movement is crucial.
Moreover, physiotherapists often delve deeper into potential contributing factors. For instance, knee-related tendinopathy might be influenced by tightness in the glutes and hamstrings. Addressing these factors through targeted exercises and stretches becomes an integral part of the rehabilitation process.
Isometric exercises continue to be a cornerstone in this phase, aiding in the reduction of pain, while concentric exercises, which involve muscle contractions leading to muscle shortening, are gradually introduced.
Concentric exercises incorporate the use of weights and engage the full range of movement, strengthening the injured area while promoting improved flexibility. Fortunately, this stage should also involve much less pain.
Long-term:
As the tendon injury progresses into the long-term phase, the focus shifts towards enhancing the resilience and strength of the affected tendon. Introducing heavier loads and varying the pace of exercises challenge the tendon and surrounding muscles, encouraging adaptability and endurance.
In this phase, the emphasis is not only on strengthening the tendon but also on enhancing joint mobility. The joint is trained to move in a multitude of ways, ensuring it can tolerate diverse loading and movements. This comprehensive approach not only promotes recovery but also helps in building a robust, adaptable tendon that can withstand the demands of daily activities and physical challenges in the long run.
By tailoring the rehabilitation process to each specific phase of the tendon injury, individuals can optimize their recovery, minimize the risk of re-injury, and regain functional abilities, ultimately improving their overall quality of life.
Strengthening Tendons, with exercises

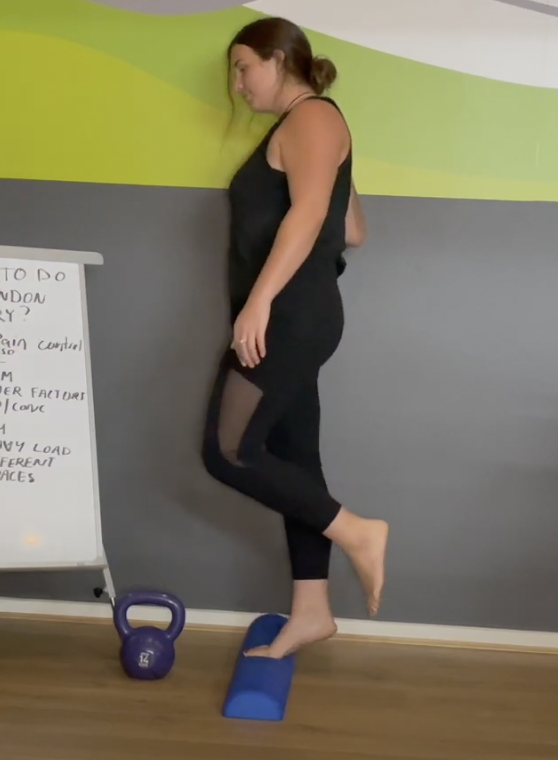
Isometric Exercises
In long-term tendon rehabilitation, it’s essential to gradually increase the weight to further strengthen the affected area. One effective isometric exercise involves using a heavier weight, such as 14kgs (adjustable based on your preference).

To perform this exercise, place the toes and the ball of one foot on a surface raised approximately 5cm high.
Lift your heel so that your foot goes beyond the neutral position.

Lift your heel so that your foot goes beyond the neutral position.

Hold this raised position for 15 to 45 seconds, depending on your comfort level.

You can modify the exercise by doing it in neutral, mid-rise, or full-rise positions, each challenging the tendon in different ways.
Calf Raises
For concentric exercises, try calf raises through the full range of movement. Lift your heel up and down for a specific number of repetitions.
This exercise can be performed at different paces; with added weight, it should be done slowly, while bodyweight repetitions can be completed more quickly.
Hopping

To further strengthen the joint and tendon, incorporate hopping exercises.
Start with one foot off the ground.

Start with forward hops, followed by hops directly upwards. These variations engage different muscle fibers and provide diverse activation. Additionally, you can incorporate multidirectional hopping, moving in various directions.
These exercises challenge the tendon’s adaptability and help build resilience, promoting a robust recovery process.
As individuals age, tendons naturally weaken, making them more susceptible to injuries that require prolonged healing periods. This concern becomes even more significant as women transition into menopause, a phase marked by hormonal changes that impact tendon health.
Engaging with a physiotherapist is crucial for a smooth and effective recovery process. Physiotherapists not only provide essential hands-on manipulations but also offer invaluable guidance on specific exercises tailored to aid in recovery.
Among these exercises, isometric and concentric exercises play a pivotal role. Isometric exercises, with their sustained muscle contractions, help in building stability and reducing pain, while concentric exercises, involving muscle contractions leading to muscle shortening, promote strength and flexibility.
By Physiotherapist Morgan Deegan
Here at Physio and Fitness Clinic, we can assist you with your sports injuries. Make an appointment with a physio today.
